Female Fertility Investigation
Endocrine Profile
Egg quality and Ovarian Reserve
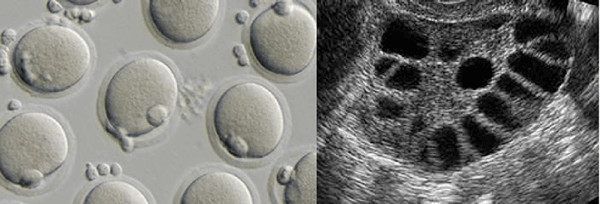
Female age is important in considering the probability for pregnancy because it is very much related to egg quality, which in turn is crucial in determining quality. Egg quantity, also referred to as ovarian reserve, is the number of eggs a woman has remaining for future reproduction. In general, egg quantity is also closely related to age, but it can vary dramatically at any age. Tests e.g. AMH are done by fertility specialists to estimate the remaining egg supply. The number of eggs obtained with IVF has a strong influence on the chance for success. Chromosomal abnormalities in eggs increase significantly with aging. Poor egg quality is often related to chromosomal abnormalities - aneuploidy. Approximately 50% of eggs produced in a women's entire reproductive history is aneuploid.
The concept of a woman's “Egg Quality” is derived from the observation that the probability of embryo implantation is strongly related to the age of the woman who provides the egg and to her ovarian reserve. Therefore, “Egg Quality” is synonymous with “the probability of embryo implantation”. Egg Quality cannot be determined by looking at the egg, measuring its receptivity to fertilization by sperm, or observing initial embryo division. Just because an embryo looks good in the laboratory, does not mean that it will implant. Just as the proof of the pudding is in the eating, the proof of Egg Quality is in the embryo implantation. Some of the noteworthy contributing factors to embryo implantation failure are Diminished Ovarian Reserve, Advanced Maternal Age and Diminished Egg Quality.
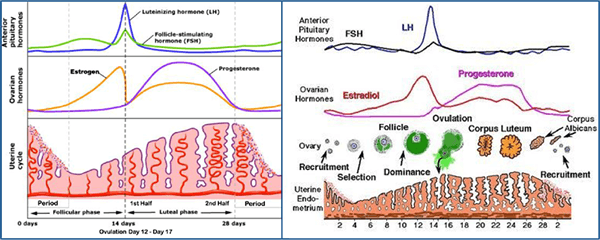
Hormone profile
Hormone tests are carried out as a part of the investigation of the infertile couple. The main ones carried out on the female are taken at a specific time in the menstrual cycle. Early or 'basal' tests are carried out on the second or third day of the menstrual period and assess function of the hypothalamic pituitary axis. These include gonadotropin (FSH & LH) and hormone levels (Estradiol (E2). If both gonadotropins and estradiol (E2) are low, then this is because the brain is not stimulating the ovaries. This is not a frequent cause of female infertility and is usually treated with gonadotropin drugs given by injection.
If the gonadotropin levels are high and the estradiol levels are low, this means the ovary is not working well (because the brain is sending high levels of FSH down to stimulate the ovary but it is failing to respond and produce estradiol (or follicles or eggs)). This is an ominous sign of ovarian function called diminished ovarian reserve. It is a cause of female factor infertility and is associated with irregular menses, infertility, poor outcomes with infertility treatment (including IVF), poor response to ovarian stimulation, and an early menopause. Unfortunately the significance of an elevated FSH level is not removed even if another test taken some months later. If the ratio of gonadotropins is reversed - that is, if the normal FSH/LH ratio is reversed - then this may be associated with a condition called polycystic ovary syndrome. This is classically also associated with elevated levels of male-type hormones called androgens (e.g.andostenedione and dihydroepiandrosterone).
Tubal Patency
Laparoscopy
A laparoscopy forms the cornerstone for the surgical evaluation of the pelvis of an infertile woman after a basic infertility investigation is completed. In some cases where endometriosis, pelvic inflammatory disease, or pelvic pain needs evaluation, it may be indicated earlier in the evaluation. The laparoscopic procedure is sometimes combined with a hysteroscopy when indicated.
Laparoscopy is performed under general anesthesia in a surgical center. A small needle is inserted into the abdominal cavity and C02 gas is introduced. The laparoscope (a telescope with a strong light and camera) is introduced through the navel. A variety of instruments can be inserted into the pelvis, through other small incisions, to perform diagnostic and corrective surgery. This procedure allows the physician to visualize the internal organs where reproduction occurs.
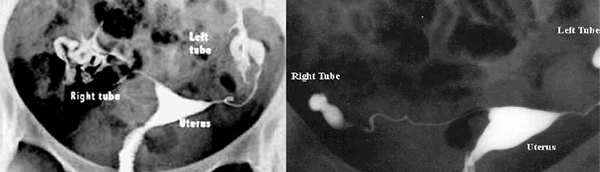
Hysterosalphingogram
A hysterosalpingogram or HSG is an important test of female fertility potential. The HSG test is a radiology procedure usually done in the radiology department of a hospital or outpatient radiology facility. Radiographic contrast (dye) is injected into the uterine cavity through the vagina and cervix.
The uterine cavity fills with dye and if the fallopian tubes are open, dye fills the tubes and spills into the abdominal cavity. This shows whether the fallopian tubes are open or blocked and whether a blockage is at the junction of the tube and uterus (proximal) or at the other end of the tube (distal).